Ambulance
Hôpital ambulant, 'walking hospital' (French, 18th c.)
Accident
You're up on a ladder, working on your Halifax house. The wood shingles need scraping before they're stained again. As you reach outward to scrape off a big flaky patch, one foot of the ladder pivots. You drop the scraper, spin to the right as the ladder goes left, and grasp at the shingles on your way down. It's all in slow motion. You remember that your hips should have stayed between the side rails. Too late now. The ladder hits the concrete driveway with a crash. You land with a thud.
Your neighbour runs over. You're in a daze. Blood oozes from the back of your head. She pulls out her phone and calls 911. It's answered by the dispatch centre at the RCMP provincial headquarters in Dartmouth, which notifies the Medical Communications Centre, also in Dartmouth. Following Emergency Health Services (EHS) criteria, a dispatcher assigns an ambulance to the call. Medical first responders from a fire station also may be dispatched. Each ambulance is tracked using GPS from this central location. For you, an ambulance at the EHS station on Agricola Street gets the call and departs for your Halifax house.

Paramedics
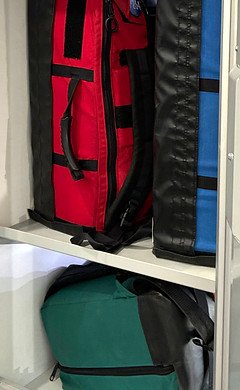
Six minutes later, the ambulance arrives. Two paramedics unload equipment kits from a compartment on the outside of the ambulance: a green backpack with essential supplies, an oxygen kit, and a cardiac monitor. Due to your fall, they also take a red trauma kit and a blue airway kit.
First, they survey the scene for any risks or difficulties. All clear. Your neighbour points to the ladder and describes what happened.
One paramedic does a primary assessment to check your whole body for injuries. She also assesses your level of consciousness, using the Glasgow Coma Scale (GCS):
-
Eye response is 3 out of 4 (You open your eyes only when someone tells you to do so.)
-
Verbal response is 3 out of 5 (You say inappropriate single words.)
-
Motor response is 4 out of 6 (When painful pressure is applied, you pull away.)
Your GCS, 10 out of 15, coupled with the mechanism of your injury, suggests a traumatic brain injury. You're breathing adequately, so you don't need breathing support. One of the paramedics wraps a bandage around your head to slow the bleeding.
Stretchers
The other paramedic returns to the ambulance, opens the back doors, and slides out a power stretcher. If you were more conscious, you'd be impressed by the Stryker Power-LOAD Power-PRO XT. Its battery-powered hydraulic system raises and lowers the stretcher at the push of a button, minimizing repetitive strain injuries to paramedics. It can support 700 pounds. EHS also has a wider bariatric stretcher for patients up to 1,600 pounds. Maybe you can watch the whole tutorial later.
Your neck or spine also may have been injured in the fall, so they use spinal motion restriction by applying a cervical collar around your neck and securing you to a scoop stretcher that slides in from both sides and clips together. They also stabilize your pelvis with a pelvic binder, in case you sustained a pelvic injury when you fell.
One paramedic attaches four electrodes to your arms and legs, then connects their colour-coded leads to a monitor/defibrillator on the ground beside you. Its digital display will continue to show your vital signs, including heart rate, blood pressure, and blood oxygen level.
The paramedics lift you onto the power stretcher, remove the scoop stretcher, and buckle you in. They attach the monitor/defibrillator to a bracket above the power stretcher, wheel you to the back of the ambulance, then attach the power stretcher to the power loader inside. With the push of a button, it elevates itself, raises its legs, then slides along a rail mounted to the ambulance floor and locks into place. Really, you'd be impressed.


ferno.ca/product/exl-scoop-stretcher/


Ambulance
The ambulance pulls away, with one paramedic driving and the other in the patient area. The one beside you applies oxygen, starts an intravenous line to administer fluid, and reassesses your condition.
With your low level of consciousness, you're missing out on this closeup view of the ambulance. The chassis is a Ford E-350 cutaway van, with dual rear wheels on each side. Tri-Star in Yarmouth added the aluminum body and the equipment to turn it into a Type III ambulance. Like all ambulances in central Nova Scotia, it's maintained and equipped at the EHS Fleet Centre in Dartmouth.
The exterior shell of the ambulance is aluminum. There are two doors at the back and one on the right side, each with a window. Four other exterior doors lead to compartments for the electrical system, oxygen cylinder, stair chair, scoop stretcher, backboard, and equipment kits.
The cab in front is outfitted with digital displays and communication equipment, plus an interior sliding window that connects the front to the back.



Inside the patient area, the walls and ceiling are gelcoated fibreglass. The flooring is non-slip vinyl. The interior is 140" long but only 66" high, so it's fortunate that no one needs to stand up. Still, the interior has yellow grab bars, plus yellow head bumpers above the doorways. Along the side walls are cabinets with clear plexiglass doors and illuminated shelves for hundreds of items. Alongside the power stretcher is a sliding chair for a paramedic, plus two fixed chairs, a workstation, and a wall kit.
The paramedic beside you radios to the Halifax Infirmary's Emergency Department to request a trauma team activation. The Medical Communications Centre monitors the conversation and alerts the trauma team when the request is approved. The paramedic tells the Infirmary your age, the time of injury, mechanism of injury, injuries sustained, your current vital signs and GCS, the treatment you received, and how soon you'll arrive. To convey information methodically, paramedics use the acronym ATMIST-AMBO as a mnemonic.
Emergency Department
With lights and siren on, the ambulance travels down Robie Street, squeezes through stubborn traffic at the Willow Tree intersection, continues to the ambulance entrance on Summer Street, then up to the portico outside the Emergency Department at the third floor level. The paramedic who was driving opens the back doors and unloads the power stretcher. Both paramedics wheel you through the entrance. You're directed through a pair of metal doors to a trauma room, where a large trauma team is already waiting.


Trauma Room
Inside the trauma room, the attending paramedic gives a brief report to the whole trauma team: your age; you fell 8 feet from a ladder onto concrete 30 minutes ago. Open head wound and suspected traumatic brain injury. GCS 10, heart rate 122, respiratory rate 20, blood pressure 151/76, pupils are sluggish. Spinal motion restriction and pelvic binder are in place. IV fluid initiated and oxygen administered.
When everyone is ready, a paramedic adjusts the height of the power stretcher, unbuckles you, and helps slide you across to the hospital's trauma stretcher.

As a Nova Scotia resident with a health card, you'll be charged $146.55 for your trip: a bargain, to be sure. Your prompt medical treatment follows comprehensive guidelines for paramedicine and owes much to Ron Stewart, a doctor from Cape Breton who pioneered on-site emergency medicine in Canada in the 1990s.